LAMPANG – Public Health Officials have asked for calm after claims of a flesh-eating bacteria outbreak. Health officials said there is no proof yet that a man who died on a bus contracted this specific infection. They are waiting for lab results before making any firm statements about the cause of death.
On Monday, a 38-year-old man from Lampang died while travelling on a bus from Nakhon Ratchasima to Chiang Mai. The bus was parked at Lampang’s main terminal when staff found him with severe leg swelling and bleeding. The hospital staff’s first report listed sepsis (infection in the blood) as the cause of death, and raised the possibility of necrotizing fasciitis (sometimes called a flesh-eating disease).
Dr Suwan Phetcharung, head of the Lampang Provincial Public Health Office, spoke to the media on Tuesday, saying the man’s wounds did not have the clear signs of flesh-eating bacteria, such as dark, sunken dead tissue in the middle of the wound.
He explained that it could be another type of infection. The health office is waiting three to seven days for test results, and is checking for all possible bacteria. Dr Suwan stressed that there have been no previous cases of necrotizing fasciitis in Lampang. He encouraged people to take care of any wounds straight away and to contact authorities if they see an unusual number of animal deaths in their area.

Flesh-eating bacteria infections
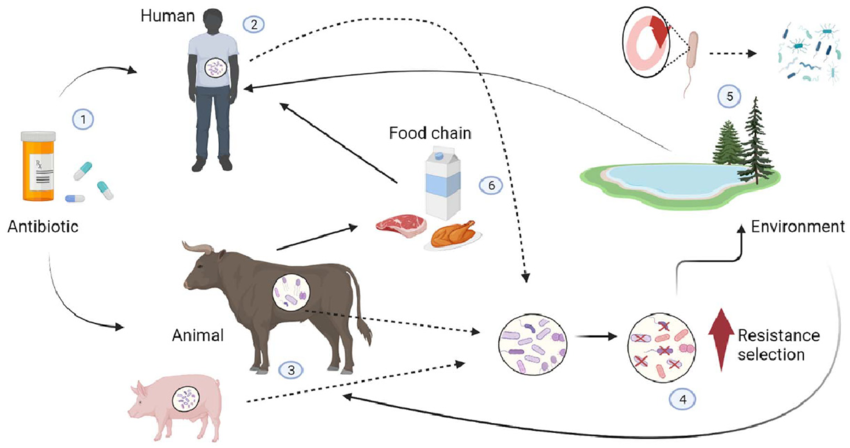
Flesh-eating bacterial infection does not spread from person to person. People usually get it from sources like animals, breathing in spores, eating contaminated food or coming into contact with dead animals. People who own pets like dogs and cats should get them vaccinated and avoid direct contact if there are any outbreaks. Any sudden animal deaths should be reported for investigation.
Symptoms of flesh-eating bacterial infection can look like common illnesses at first. It may cause a runny nose, fever, or shortness of breath if it affects the lungs. It can also cause stomach pain, nausea, and diarrhea. On the skin, there may be rashes, blisters and eventually a dark, sunken centre in the wound. So far, these symptoms have not shown up in Lampang.
Doctors have confirmed that the man died from sepsis and necrotizing fasciitis. There is no evidence yet to say it was caused by the bacteria known for flesh-eating disease in humans. Many types of bacteria can cause necrotizing fasciitis, such as group A streptococcus and others.
Bacteria can enter the body through cuts or wounds. Infections often cause swelling, redness, pain and tenderness at the site. If the infection spreads, the skin can turn dark purple within 36 hours, sometimes with blisters. The bacteria may reach deep tissues and muscles. Without quick treatment like antibiotics or surgery to remove dead tissue, the infection can spread to the bloodstream and become life-threatening.
Bacteria can spread from animals to humans
People at higher risk include those with chronic illnesses like diabetes, skin conditions, low immunity from steroids, cancer or diseases affecting the kidneys or liver. The health office recommends people stay alert for new or worsening wounds, fever and pain. Early treatment at the nearest clinic or hospital can save lives.
If a serious bacterium like anthrax is found, extra care must be taken with animals, as some diseases can spread from animals to people. Authorities are still waiting for lab results to confirm which bacteria were involved in this case. Dr Suwan said people shouldn’t worry too much at this stage. The wound could be from another infection, as deep tissue infections happen from time to time.
In the last two or three years, Lampang has seen only a small number of these cases, usually related to delayed treatment or when the infection has already spread to the bloodstream. Early treatment with antibiotics and surgery is effective in most cases.
In recent years, Lampang has not reported any confirmed cases of flesh-eating disease. More common are skin infections from injuries like stepping on a nail or untreated wounds. These can also lead to serious problems if not managed early.
In 2024, there were two deaths from skin infections among outpatients and 13 among inpatients. Most of those who died had other health problems such as diabetes, weakened immunity or advanced age.